MY TAKE ON COVID 19
I wrote this after extensive research, my experience as a physician with 30 years experience in a a family practice setting and some common sense. I hope you can all learn something, as I certainly have. I update this post daily depending on new information widely available.
As we learn more about this virus, the key issue has become the method of spread. It was not until May 20 that it became accepted that it is spread by aerosol making it extremely contagious. When I first started the post on April 12, this was my main contention.
Little has been added to this post since July 2020, but it is still accurate.
MAJOR POINTS
1. COVID-19 is here to stay. Like past major viral diseases (smallpox, polio, measles, rubella, mumps,, chickenpox) and bacterial diseases (diphtheria, whooping cough, tetanus) – ie all the diseases we now control with vaccines, it will only be controlled by excellent public health and a vaccine that will produce long-lasting immunity. Along with naturally acquired infection, herd immunity is necessary for control in any population.
We have to follow the example where excellent public health has been successful: South Korea, Taiwan, China, Hong Kong and Singapore. Even here, outbreaks continue to occur. In these countries, most businesses have remained open. They all learned a lot from the SARs and MERs epidemics and instituted effective measures early in the pandemic.
Not doing this will only result in second, third and more waves of infection.
2. Masks. I first stated on this post on April 14 that COVID-19 is a respiratory virus primarily spread by aerosol and small droplet spread, not by large droplets that settle on surfaces that are then spread to our mouth by our hands. A major mistake has been the emphasis on hand washing – not a bad idea and still of general value – but by thinking that this was sufficient, it produced overconfidence as the method that would prevent spread. Hand washing only produces eczema and the vast overproduction of hand sanitizer.
The deemphasis on using masks has been disastrous. There is a huge pool of asymptomatic “silent spreaders” – those in the 2-7 day incubation period and the 50-60% who never develop symptoms – that will continue to spread the infection. From the evidence from Vo, Italy and the aircraft carrier USS Theodore Rosevelt – where 100% of people were tested with 53% and 60% completely asymptomatic respectively – this spread is prevented by masks.
A major problem are the 20 somethings (coronaenialls) who because they are at low risk are not practicing distancing and not wearing masks. Children are probably also significant silent spreaders. Pets, especially cats, may even be a source.
Masks should be mandatory for anyone going out in the public and fines should be instituted for not following the rule. Masks probably do not work as well to prevent acquiring the infection. Common sense is necessary – masks are not necessary when you are isolated – driving in your car, inside your house or outside with no one around.
3. Testing. As COVID-19 is so often asymptomatic, frequent testing is mandatory. Taking temperatures is not of much value in ruling out infection because of the 2-7 day incubation period and asymptomatic people. Testing facilities would need to be scaled up significantly. Drive in testing facilities should be everywhere.
Testing consists of direct methods to detect the virus or serological tests to detect the antibodies produced by infection.
4. Public health. This pandemic will only be controlled by good public health practices. All positive cases and anyone with typical symptoms must be quarantined and all their contacts traced. Contacts also need to be quarantined until tests are negative. This should be a combination of traditional tracing done by “boots on the ground” requiring an army of “volunteers” to deal with the immense job, and the use of apps to track the contacts of those infected.
5. Apps mandatory for everyone. Apps on everyone’s phone should likewise be mandatory. With so many cases, how else do we institute contact tracing and enforce physical distancing? This is the digital age and it amazes me how slowly we have been to institute simple technical methods as has been done in Singapore, China, Taiwan and South Korea.
There are two main types. Apple/Google have produced an app where the information remains on everyone’s phone, is anonymous and completely private. Blue tooth is used to detect location.
The other is to require all to register with central agencies and allows proper contact tracing. To go back to work or function normally in public, one would have to show their app proving they are not infected. “Passports” could be issued showing lack of infection. China uses codes to indicate status: green (no disease, no infected contacts, very recent negative test, positive serology indicating immunity, recovered from the infection), yellow (contact with infected people but status uncertain) or red (symptoms, proved infection).
Many have complained that this would be an invasion of privacy. However, this is little privacy now with all the digital info obtained by Facebook, Google, Amazon and multiple other agencies. But in times like this, this seems like a minor price to pay. It entails that we trust the owners of the information – the government would use the information in a responsible way.
These would only be an adjunct to testing. It is estimated that at least 60% of the population would need to be using the app to be effective. It should be mandatory.
6. Physical distancing and loosening self isolation. Still mandatory when around others (I think the 2 metre rule should be lengthened), some common sense must be instituted. Keeping people inside for the long period that will be necessary for control – ie until a vaccine is generally available (estimated to be 12-18 months) will produce serious social consequences. Why can’t a family take their kids to a park and let off steam? Other common sense places include golf courses, tennis courts, parks (municipal, provincial and national), beaches etc. The economic effects will dominate society.
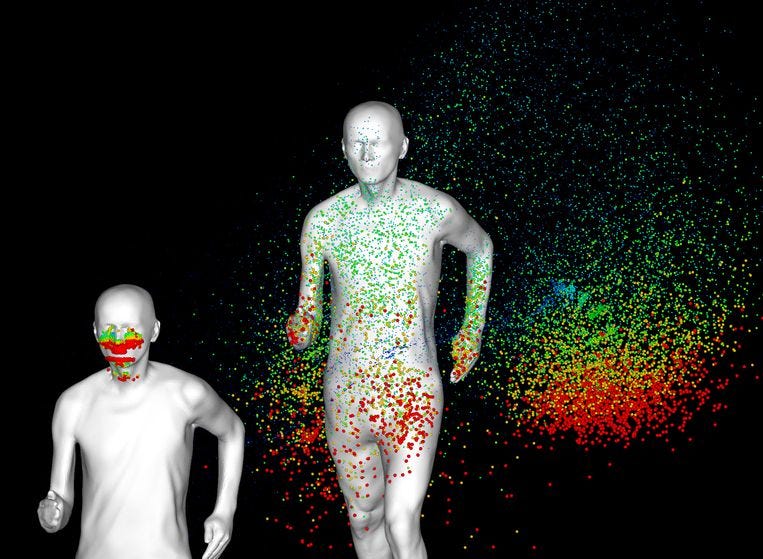
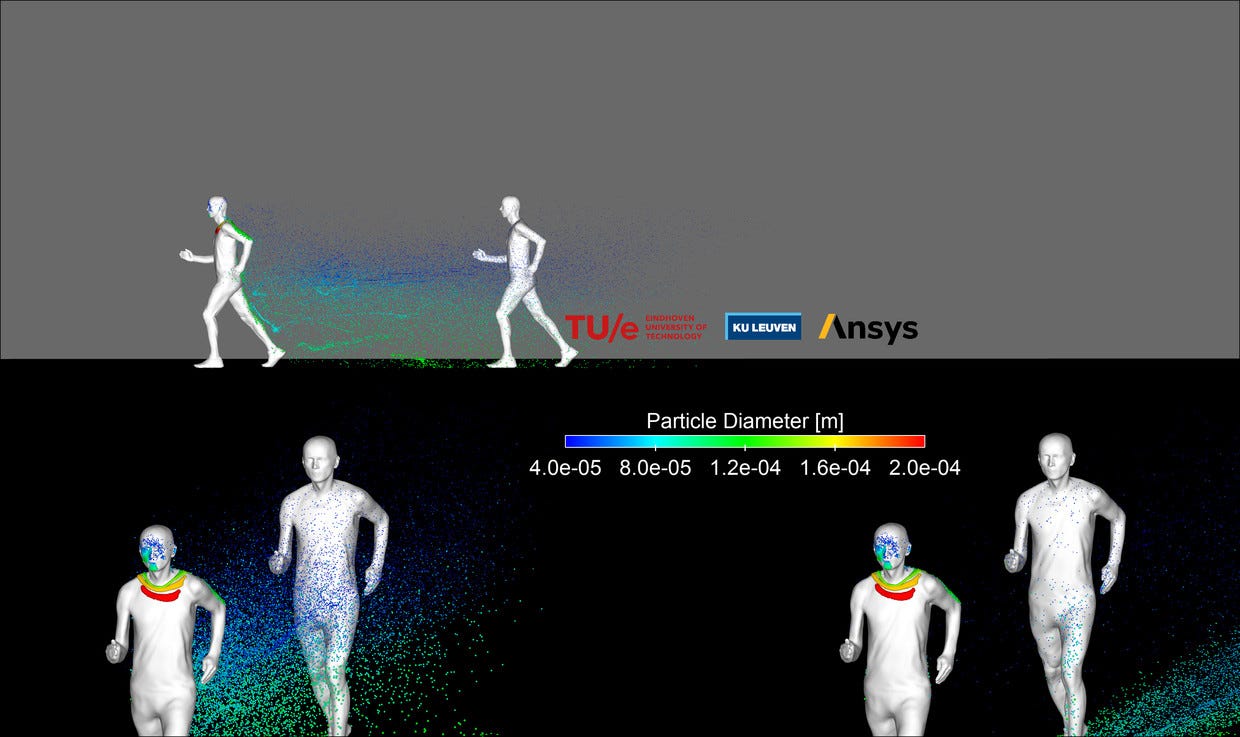
Beware of the jogger or cyclist moving past you. Their breath slipstream travels for many yards.
7. Open the economy as soon as possible. After effective public health measures are in place, economies have to return to normal quickly.
The economic and social costs of lockdowns are enormous: estimates suggest that every month of pandemic-related restrictions will shrink the economies of advanced countries by two percent. All western countries will see their economies shrink by more than 25 percent within a year. Unemployment is rising to levels unheard of since the 1930s—fueling political backlash and deepening social divisions.
Lockdowns are simply not sustainable for the amount of time that it will likely take to develop a vaccine. Letting up will reduce economic, social, and political pressures. It may also allow populations to build an immunity that will end up being the least bad way of fighting COVID-19 in the long run.
The justification for general lockdowns grows weaker and weaker. The cost of protecting at risk populations is much lower than forcing everyone to stay home. Countries need to realize that managing—rather than defeating—the pandemic is the only realistic option. At the end of the day, increased—and ultimately, herd—immunity may be the only viable defence against the disease, so long as vulnerable groups are protected along the way.
THE VIRUS
In late December 2019, the first cases of a pneumonia of unknown origin were identified in Wuhan, the capital city of Hubei province. Wuhan, with a population of 11.08 million people is the most populous city of central China and the 9th most populous in the country. The disease spread rapidly throughout China causing varying degrees of illness. Patients often presented without fever, and many did not have abnormal radiologic findings.
The pathogen was identified as a novel enveloped RNA betacoronavirus that was initially named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has a phylogenetic similarity to SARS-CoV. COVID-19 is the colloquial name given to the organism. COVID-19 is a RNA virus, a collection of genetic material packed inside a protein shell.
COVID-19 is a novel virus to which nobody has immunity. Much is unknown and knowledge has been slow to accumulate. It is extremely contagious with a contagion rate (R-rate) of 2.5 – 3 – without quarantines and social isolation, everyone infected passes it to 2+ others – an exponential rate that results in rapid escalation of the disease. However this R rate applies to early stages of the epidemic and decreases as more people get infected and are immune and as preventative measures are enacted. It is thought that the R rate needs to be less than 1 for control and loosening of restrictions.
As many as 50+% of those infected are asymptomatic but because of inadequate testing the actual numbers are unknown. These asymptomatic people shed the virus and quite likely are the most common vector.

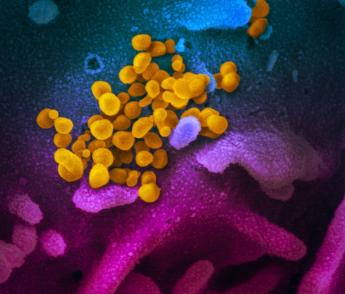
This scanning electron microscope image shows SARS-CoV-2 (yellow), the virus that causes COVID-19—isolated from a patient in the U.S., emerging from the surface of cells (blue/pink) cultured in the lab.

SIGNS and SYMPTOMS
Respiratory viruses initially infect the nose and throat and then the lungs potentially causing a viral pneumonia and COVID-19 follows this rule. After a mean asymptomatic period of 4 days (range 2-7), fever, chills, headache, muscle aches, loss of appetite and malaise/fatigue start. These symptoms seem to last unusually long, often for 2-3 weeks or more, and can be severe. Physical exertion is difficult. 20% experience loss of taste and/or smell and some have a variety of skin manifestations. Progression results in a dry cough, shortness of breath and a viral pneumonia that can progress to respiratory failure and life-threatening complications, including acute respiratory distress syndrome, multi-system organ failure, and ultimately, death.
In the absence of a proven effective therapy, current management consists of supportive care, including invasive and noninvasive oxygen support. In addition, many patients have received off-label or compassionate-use antiretrovirals. With respiratory failure, the only supportive therapy is mechanical ventilation. This requires intubation – an endotracheal tube inserted into the trachea – 100% sedation to tolerate it, and attachment to a ventilator that breathes for you. At this stage, survival is only 10-30%.
The New England Journal of Medicine extracted data regarding 1099 patients with laboratory-confirmed COVID-19 from 552 hospitals throughout mainland China through January 29, 2020. Patients were both in- and out patient. The end point was admission to an intensive care unit (ICU), the use of mechanical ventilation, or death.
The median age was 47; 41.9% were female. The end point occurred in 67 patients (6.1%), including 5.0% who were admitted to the ICU, 2.3% who underwent mechanical ventilation, and 1.4% who died. Among non-residents of Wuhan, 72.3% had contact with residents of Wuhan, including 31.3% who had visited the city. The most common symptoms were fever (43.8% on admission and 88.7% during hospitalization) and dry cough (67.8%). On admission, ground-glass opacity was the most common radiologic finding on chest computed tomography (CT) (56.4%). No radiographic or CT abnormality was found in 157 of 877 patients (17.9%) with non-severe disease and in 5 of 173 patients (2.9%) with severe disease. Lymphocytopenia (a low white blood count, typical of most viral infections) was present in 83.2% on admission.
As there are more cases, general systemic complications are being documented.
Thrombosis. Investigators in the Netherlands found a “remarkably high” 31% rate of thrombotic complications among 184 critical care patients with COVID-19 pneumonia. Inflammation in the blood vessel walls may be driving thrombosis formation. Venous thrombosis, pulmonary embolism, arterial thrombosis and stroke are the most manifestations. Acute, large vessel strokes in COVID-19 patients under age 50 years (a sevenfold increase in what would normally be expected) are also occurring.
All ill patients, even those not in the ICU, should receive prophylactic-dose low molecular weight heparin (LMWH), unless they have contraindications.
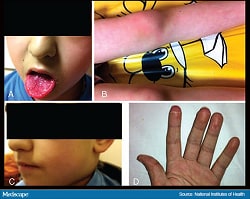
Pediatric Multisystem Inflammatory Syndrome. (Kawasaki-like disease or Mucocutaneous Lymph Node Syndrome). Kawasaki disease is a post viral syndrome that had been described for decades and in this pandemic, was first described in Britain, 25 patients in France and by mid-May, 200 cases in 18 US states but was not seen in China nor Japan. Three died in the initial 85 US patient cohort (plus 2 others possibly related).
It presents with a persistent fever, lymphadenopathy, a characteristic skin rash, glossitis (strawberry tongue), conjunctivitis, abdominal pain and an unwell child. An arteritis involving the heart’s coronary arteries, kidneys and other organs is the most serious complication and is what causes death.
Few tested positive for COVID-19 by swab tests but many are positive by serology indicating a late onset after the infection. This is considered to be a “post-viral” syndrome with an onset around 4 weeks after acquiring COVID-19. The patient’s immune response to COVID-19 is the underlying mechanism.
Treatment consists of supportive care, anti inflammatories, cortisone and immunoglobulin
It should be emphasized that this is rare but shows that no one is spared in this infection.
Cardiac disease. COVID-19 activates the renin-angiotensin system and this may explain why patients with hypertension and heart failure (more often men) do worse with COVID. Angiotensin inhibitors or ARBs are used to treat hypertension and heart failure and have a beneficial effect in preventing complications.
Skin manifestations:
• Idiopathic pernio. Acral erythematous to violaceous papules, plaques, pustules and vesicles primarily affecting the toes and less frequently fingers mimicking chilblains (19%). In 59% of these patients, this developed after other symptoms., and was correlated with a milder disease course and younger patient age. This tends to be more severe and symptomatic (itching, burning, pain), is more likely to ulcerate, and takes longer to resolve than other skin manifestations. .
• Vesicular (chicken pox-like) eruptions (9%). These appeared earliest in the course prior to any other symptoms in 15% of cases. These developed on the trunk and extremities, were most common in middle-aged adults, and typically lasted around 10 days.
• Maculopapular eruptions (47%). Seen in more severe infections and appeared at the same time as other COVID-19 symptoms.
• Urticaria (19%)
• Livedo or necrosis (6%). Indicates more severe illness and a poor prognosis.
Seasonal Course? Some corona viruses, especially influenza, have a seasonal course – influenza and the common cold are almost always more common in cold seasons and tend to disappear over the summer. This is because, in dry cold air, the water component of the droplet is minimal and the virus spreads faster. Other factors like closer contact inside houses etc. in cold seasons also play a role.
In the 1918 influenza pandemic, the initial course was in the spring, disappeared over the summer and then reappeared in the fall but in the 2009 H1N1 epidemic (the same virus in the 1918 epidemic), it still spread in April and May. It is not known if COVID-19 will lessen in the summer. It seems unlikely as it is common and spreads actively in warm places like Singapore. Read the fascinating book “The Great Influenza” to understand influenza and pandemics.
SOURCE OF COVID-19
It is very likely that it originated in wild animal markets in Wuhan. Though the exact source is unclear, bats are the most likely. Chinese don’t eat bats or make “bat soup”. Bats probably spread it to other mammals and thence to humans. These “wet markets” serve as the primary food source for most Chinese. See the post Wet Markets to understand what they are like.
/cdn.vox-cdn.com/uploads/chorus_image/image/66656302/GettyImages_1203053955.0.jpg)
In Wuhan, snakes, raccoons, dogs, porcupines and deer were just some of the species crammed inside cages, side by side with shoppers and store owners. Some animals were filmed being slaughtered in the market in front of customers.
Wild animal products form an important part of traditional Chinese medicine practiced more than traditional Western medicine in China.
It is also very clear that other mammals can get (and probably then spread) this virus. Three tigers and one lion in the Bronx Zoo have been infected. They developed lethargy, loss of appetite, fever and a cough and all measured positive for the virus. It has been suggested that cats are more likely than dogs to be vectors
Two New York cats became the first confirmed pet cases of COVID-19 in the United States in late April. The cats, who live in different parts of the state, are believed to have contracted the virus from people in their household or neighbourhood. One pug in Georgia tested positive.
While there have been other cases of pets contracting the virus from people, there is no evidence that pets can then transmit COVID-19 to other people, but there is no reason why they wouldn’t. I would exercise caution with your pets – this extremely infectious disease is spread by aerosol and there is no reason why pets are not another “silent spreader”.
IMMUNITY AND MUTATIONS
The complete viral genome was sequenced within two weeks in mid January. Many new strains have been detected. RNA viruses, like influenza and measles, are more prone to changes and mutations compared with DNA viruses, such as herpes, smallpox, and human papilloma virus (HPV). RNA viruses are expected to change frequently and this virus is no exception. The new copies are not far off the original virus. The varieties in Italy and New York are not more infectious or fatal than the original strain that appeared in Wuhan, China in late December. Nearly all mutations will make some part of the virus work less well and these “inferior” copies die out quickly,
Vaccines tend to target early versions of the virus that preserve enough features to provide immunity against most variants.
The flu virus mutates fast and erratically from year to year.As our immune system has a bad memory for flu viruses – the immune response to the flu only lasts around a year before we need to get revaccinated.
A better analogy for COVID-19 are measles, mumps, and rubella (also RNA viruses) for which we have had effective vaccines for decades. Thus, it should be possible to make an effective COVID-19 vaccine that will provide long-lasting immunity just as we have for many other viruses that do not change rapidly. Even if random mutations do occur down the road, the worst-case scenario is that we’ll see some breakthrough infections, but we wouldn’t have breakthrough life-threatening disease.
It’s still unclear exactly how long immunity lasts once a person’s immune system beats the infection. In the SARS pandemic in 2003, people who had SARS had a strong supply of SARS antibodies for about 2 years, providing immunity, but after about 3 years, those SARS antibodies tapered off, and people had a higher chance of contracting the virus again. The timeline with COVID-19 antibodies may be similar.
Within a few years, we’ll hopefully have enough herd immunity — from a vaccine along with natural immunity from so many people contracting it — to have eradicated the disease so reinfection will no longer be an issue. Vaccines confer memory so a subsequent infection will still tend to elicit a favourable immune response.
In April, South Korea reported 91 patients thought recovered, who tested positive again. These were unlikely reinfections, reactivation or relapsed bur were shedding the viral remnants and probably not infectious. False test results could also be at fault.
SPREAD
Asymptomatic Spread. It is very clear that this virus is actively spread when infected people are asymptomatic, both during the 2-7 day incubation period and in those who never develop symptoms. As a result, depending on temperatures for screening misses
50-60% of those infected.
One study that is getting surprisingly little press occurred in Vò, Italy, a town near Venice with 3000 citizens – and where the first death in Italy occurred on March 6. The town was immediately quarantined and all 3000 were tested for infection. There were 89 positives, 53 of whom were asymptomatic – and significantly most of these remained asymptomatic. All positives were quarantined and all 3000 were tested again 9 days later. There were 8 positives with 5 being asymptomatic. They were able to completely control the epidemic in under 14 days.
The aircraft carrier Theodore Rosevelt is another glaring example of asymptomatic spread. All 4,900 sailors were tested with 1000 positives, 60% of whom were asymptomatic – and remained asymptomatic. Only one died. The Anderson Cooper interview of his wife on CNN was heartrending, especially as Anderson kept crying.
This emphasizes that masks (that work well to prevent an infected person from spreading the disease) should be mandatory for anyone in public.
Method of spread. Corona viruses are respiratory viruses like SARS, MERS (both corona viruses), influenza, and the common cold (over 100 different viruses, including some corona viruses). Respiratory infections are spread by aerosol and droplet spread primarily. No matter what we like about this, when we speak or exercise, we constantly expel droplets of saliva that contain the virus. Several studies have shown this.
1. Aerosols of virus. As virus is aerosolized constantly with normal speech and simple exhalation, simply sitting at a table with others is likely to cause significant exposure. A study done by the National Institutes of Health in the US and released on May 15 involved spraying a florescent dye into subjects mouths. They then breathed into a special “box” with UV light. It showed that many particles remained suspended in the air at 7 minutes and in some lasted 14 minutes. This helps explain the extreme contagiousness of COVID-19. Despite months of denying, aerosol has become the primary route of transmission between people. This reinforces the importance of masking.
These droplets can contain respiratory pathogens such as Mycobacterium tuberculosis, influenza viruses, and measles virus. Fecal–oral is not a method of spread.
To measure the size of droplets emitted through speech, they used an intense sheet of laser to visualize bursts of speech droplets produced when subjects said the words “stay healthy.” The method is particularly sensitive in detecting speech droplets with diameters of less than 30 μm, which could remain airborne far longer than the larger droplets that have typically been the subject of research. It was estimated that one minute of loud speaking generates at least 1000 droplets capable of carrying virions — units of the virus that can cause infection. The droplets remained airborne for 8 to 14 minutes, long enough for someone to inhale them and become infected. Droplet nuclei averaged 12 to 21 μm in diameter when first emitted and 4 μm after drying in the air, and that a 10-μm droplet has a 0.37% probability of containing at least one virion.
Shouting, singing, coughing and sneezing produce exponential increases in the number of virions emitted. A May, 2022 study showed that people doing high-intensity exercise in gyms released 76,200 aerosol particles per minute.

Expulsion of virus in saliva droplets. Vigorous “spitty” speech, a cough or sneeze expels many times more droplets that from the force of expulsion, can travel long distances. That formed the basis of maintaining the 6 feet or 2 metre (actually 6½ feet) distancing. A JAMA article suggested that 24 feet was a better distance to prevent spread. Florescent dye sprayed into mouths (and then coughed) or placed on one person’s hands has shown that the dye is spread literally everywhere in a room.
Transfer from contaminated surfaces. Larger droplets of saliva settle out on surfaces and this was initially suggested as the primary cause of spread. The virus lasts about 24 hours on cardboard and 3 days on plastic. In hospitals, the highest concentration of virus is in toilets and personal protective equipment removal rooms. This resulted in the recommendation to not touch your face and that hand washing for 20 seconds (how long it takes to sing “Happy Birthday”) were all that was necessary.
But this has done little to control spread, produced a lot of hand eczema and the overproduction of hand sanitizer.
I believe that spread by aerosol by far the major cause of spread – and as a result, wearing masks correctly is of much more value than hand washing. As all early recommendations only emphasized hand washing, this has resulted in the exponential spread of COVID-19 and has been disastrous.
Fecal-oral spread. People with COVID-19 often have gastrointestinal (GI) symptoms such as diarrhea, and a lot of SARS-CoV-2 RNA has been detected in their stool specimens. In a study released on May 13 in Science Immunology, high levels of viral RNA were found in three of ten samples, but no virions were seen in any of them.
Finally, they bathed the virus in various simulated human gastric and intestinal fluids. In contrast to the rotavirus, which is transmitted by the oral–fecal route, SARS-CoV-2 “lost infectivity” in the low pH simulated gastric fluid within 10 minutes. It was “inactivated” by components of human colonic fluids, decreasing by fivefold within an hour. It was theorized that SARS-CoV-2 replicates in human intestinal enterocytes, but then is inactivated in the lumen of the colon. The finding means that toileting is not a particular concern for this virus and that ingestion with food is of little risk.
Prolonged viral shedding. In a small study of 56 convalescing patients from Wuhan, it was shown that viral shedding occurred at the following rates: at week one (100%), followed by 89.3%, 66.1%, 32.1%, 5.4% and 0% at weeks two, three, four, five and six, respectively. However, similar to other virus infections, this is not indicative of the transmission ability of the infected individual. Patients with longer viral shedding tended to be older and were more likely to have comorbidities such as diabetes and hypertension.
This is the most likely cause of patients testing positive after having recovered from COVID-19.
PREVENTION OF SPREAD
a. Early testing, quarantining of positives and contact tracing. The experience in China and Vô, Italy showed that aggressive early action is the only way to control COVID-19. Public health measures are going to be the way the disease will be controlled until an effective vaccine can be administered to enough citizens to establish herd immunity.
The government could identify and isolate clusters, quarantine everyone affected, trace their recent contacts, and quarantine and isolate them too – whether they had symptoms or not. Most contact tracing has a heavy manpower requirement that is easily overwhelmed when an epidemic is out of control. As a result an army of volunteers and using apps that trace people that were contacts of people with the infection and then notifying them is of much more value. Some work on location of phones and others on GPS with is of less value in evaluating distancing techniques. We are in a digital age and technical methods like this were shown to be of great value in China, Singapore, Taiwan and South Korea.
This demonstrated a valuable principle: testing of all citizens, whether or not they have symptoms provides a way to control this pandemic. Establishing a structured response like this is key, and widespread testing is crucial in telling an accurate story of how many people are affected, and what the mortality rate of the virus actually is. On first examination, this seems costly but in fact is may be cost effective as numbers stay low. The long-term effect on economies would be minimal. A robust public health system is necessary.
At the time of the Vô experience, this approach in large Italian cities where infections were out of control was impractical but would have been possible early almost everywhere else in the world before the crisis became uncontrollable.
b. Physical distancing. As above, at least 2m from anyone not living in the same household is the minimum. However with the aerosol spread lasting several minutes, this may be insufficient. JAMA recommended 24 feet very early on.
A study in Belgium and the Netherlands showed that simply walking behind someone jogging or riding a bicycle is a significant method of spread as exercise causes you to expel many more saliva droplets than when at rest. These end up in the slipstream trailing behind the exerciser. The droplets fall but can land on clothing. On the basis of these results, they advised that for walking, the distance of people moving in the same direction in one line should be at least 4–5 meters, for running and slow biking it should be 10 meters and for hard biking at least 20 meters. Also, when passing someone it is advised to already be in a different lane at a considerable distance e.g. 20 meters for biking.
b. Hand washing and not touching your face.
c. Limiting group size. This varies from 10 to 2 combined with physical distancing. 24 feet may be necessary to prevent spread from coughs or sneezes.
d. Self Isolation and stay at home orders. Simply staying at home with no exposure to the outside except for emergencies, groceries, going to pharmacies or obtaining medical care. Exercising outdoors and walking dogs are usually allowed.
e. Quarantine. Anybody who is infected (asymptomatic or symptomatic) must limit any exposure to anyone, leave only for emergencies and wear masks when out of their house.
In Wuhan province of China, the total lockdown lasted 76 days before the rules were slowly relaxed. In a country of 1.4 billion with most of them in the eastern half of the country (most of western China including Tibet is desert or high plateau and sparsely populated), it is amazing how effective their methods were. But few counties could enforce the necessary rules as in China, a total autocracy with files already present on all 1.4 billion citizens and extensive use of apps. The Chinese population is very obedient because of severe enforcement. Chinese (and most East Asians) are also used to wearing masks and all citizens adopted this early.
Using phone apps to enforce compliance and control populations can be effective in location sharing and contact tracing. In some countries, permission to leave your house is required and is relayed by apps. Many countries have enforced these rules – fines and imprisonment are not uncommon for people not practicing distance isolation or quarantine orders.
f. Lockdown and institutional emergency orders. Virtually every government in the world has imposed lockdowns and imposed states of emergency. All nonessential businesses are closed. But more common sense needs to be exercised. There are many places and activities where physical distancing is easy and pose little additional risk: municipal, provincial and national parks, golf courses, beaches, and many more.
Borders are closed for all non-emergent or essential travel. Trucks carrying goods are the main things allowed to cross borders.
g. Personal protective equipment (PPE – masks, face visors and hazmat suits) are mandatory in health workers dealing with COVID-19. Access has been much less than desired and these heroic workers risk their lives every day. Many have died. Governments have ended up in bidding wars trying to procure adequate PPE. The US initially banned exporting PPE to Canada. PPE has been in desperately short supply everywhere.
11 million N95 masks shipped to Canada from China were defective and had to be returned.
After every patient contact who has the disease, the entire “outfit” must be changed. Removing PPE is a laborious process – after each piece is removed, the outside of the PPE is not touched and hands must be sanitized.
h. Masks. Given the evidence, universal face masking is an easy and effective way to limit the spread of COVID-19. Masks are more effective in preventing an infected person from spreading the virus than they are in preventing obtaining the infection. Larger saliva droplets are trapped much more effectively than aerosolized viral particles as the water content of the droplets decreases droplet size. Beards may decrease the effectiveness of all masks.
Masks were in early use in Asian countries and some western countries (like the Czech Republic) but a late adoption in the rest of the world. This is one of the major mistakes made in controlling the spread and I was personally very surprised when all initial recommendations were to avoid masks. Experts have feared that this would leave fewer masks necessary for health workers. Several health authorities who were previously anti-masking have now changed their tune, including the US-based Centres for Disease Control. Generally, when a pandemic is on, something over your mouth is better than nothing over your mouth. An impromptu face covering is an imperfect seal that will still allow plenty of virus-saturated air to escape, but what you’re doing is limiting the size of the virus cloud around you. The mere act of putting a barrier in front of your face dramatically limits your ability to spew water droplets into the surrounding environment.
Although two meters is recommended as the minimum social distance to prevent transmission of the virus, it’s nowhere near enough space if someone is coughing, sneezing, yelling or just happens to be a particularly spitty talker. What an impromptu face covering does is help contain a person’s viral expectorations within their two meter bubble.
The reason we’re all self-isolating, of course, is because any one of us could be infected with COVID-19 right now and not know it. Upwards of half of all COVID-19 cases don’t show symptoms. So we all have to act as if every breath out of our mouths is a potentially deadly vector for disease. As a result, anything you put in front of that mouth necessarily risks becoming absolutely saturated with coronaviruses.
The first rule of masking is to avoid wearing it if you don’t have to. If you’re in your car, home, paddle boarding or on a remote hike, your mask is best left off your face. The second rule is to be very wary of touching that mask. There are guidelines on how to properly don and doff a mask, and the gist is that you should be thoroughly washing your hands before and after putting it on. Remember that your mask, while helpful at protecting you and your community, is also a viral sponge, so treat it with the respect you would accord to any object potentially dripping with infectious disease.
There are many kinds of masks.
N95 masks are effective in both preventing spread and getting the virus and use has been reserved for medical personnel. These medical-grade masks are desperately needed by healthcare workers. They are uncomfortable wearing for long periods. N95 masks can be reused (preferably by the same person) after sterilization using UV sterilizers. Face shields and hazmat suits are also part of routine medical care of infected patients. A simple face visor can be used by threading the arms of glasses through the holes of letter sized, clear plastic document holders.
Ordinary surgical masks are less effective in preventing infection.
Anything fabric over your mouth probably has value (at least to prevent an infected person from spreading the virus): tightly woven 100% cotton fabric, a bandana, t-shirts, a scarf or even a reconfigured bra. Instructions for making a huge variety of homemade masks are available from online videos. Make one in less than a minute using only an old t-shirt and two rubber bands. A tighter, more comfortable fit can be assembled from a square of cloth, a paper towel, a length of string and a few staples to hold it all together. The Centres for Disease Control has published instructions for another “no sew” mask that involves little more than a t-shirt, a pair of scissors and about five minutes. Another uses one square and two thin strips of fabric, fold some pleats all sewn together. Sew a piece of metal, such as a paper clip, into the top seam in order to bend the mask around your nose. Patterns from fashion designers are “fashionable”. Whole groups of ordinary citizens handy with a sewing machine produce masks.
i. Leadership. The World Health Organization (WHO) has had a commendable response to and most national governments have shown poor leadership. At no other time have their importance in showing the way more important. Conservative governments (US, Brazil, United Kingdom, Russia) are more likely to institute inadequate measures until too late. Many provincial/state governments make most of the important decisions resulting in disparate responses. In the US, 50 states each have separate protocols. States with Republican legislatures and governors have been very slow to adopt advised rules with 15 states as of April 10th not instituting stay at home rules.
Countries known for their propensity to not follow rules (Spain, Italy, US) have had the most severe infection and death rates.
All public health officers and “experts” in Canada has been an embarrassment. They have showed no common sense by simply parroting distancing guidelines and self isolation that we have all heard a million times rules, but no innovation. The most glaring mistake is not mandating compulsory masks by denying that it is possible for this virus to be spread by aerosol.
Of course the idiot Trump has been completely incompetent in so many ways to enumerate here.
j. Sniffing dogs. Dogs have been trained to detect diseases like prostatic cancer and diabetes. Socks are an especially good material to use but masks from those with active COVID are used. Dogs have the advantage of being able to screen high volumes of people, up to 250 people per hour.
RISK OF DEATH
The exact incidence is difficult to determine exactly with 100% testing the only way to know it exactly. The initial very high 8% death rate in Italy belied the actual incidence as only people with symptoms were being tested. Full testing would give a clearer picture of how many people actually have the virus, and how many pass it on. As a result, actual mortality rates vary from 1.5-3% when all are tested and asymptomatic people are included.
Physicians most likely to be exposed are emergency room doctors, anesthesiologists and surprisingly ophthalmologists. The Chinese physician who first alerted the authorities in Wuhan, and subsequently died, was an ophthalmologist.
The people who do worse are:
a. Age. Risk increases with age. Young children rarely die although the emergence of . Death is most significant over age 60 increasing progressively.
My impression is that 20 somethings and teenagers are not doing as good a job and will remain a significant vector for COVID-19 and have been labeled corona-enialls. They are the “silent spreaders” in this pandemic that will only be controlled by testing everyone in a population.
b. Males are about twice as likely to die as women making up about 70% of all deaths consistently all over the world. The exact reason is unknown but men are less likely to wash their hands or follow other protective measures, have more comorbid conditions and are more likely to smoke. COVID-19 activates the renin-angiotension system worsening heart diseases like heart failure of hypertension, both more common in men. ACE inhibitors and ARBs have a beneficial effect.
A study in mice shows that estrogen protected male mice (relevance to humans uncertain).
c. Blood group A. Although present in about 31% of the population, 38% of deaths in China had type A.
d. Comorbidity – Nearly 90% of patients admitted with COVID-19 have a comorbid medical illness: hypertension (49.7%), obesity (48.3%), chronic lung disease (34.6%), diabetes (28.3%), and cardiovascular disease (CVD) (27.8%). The mean age of patients in Italy who died from COVID-19 was 81 years and older, and more than two-thirds of persons who died had comorbid conditions of diabetes, CVD, or cancer.
There are multiple pathways lead to greater COVID-19 morbidity and mortality in persons with diabetes. 1. Ample data show that people with diabetes are more prone to infection, hospitalizations, and premature death if not properly treated. Viral infections are said to be a major cause of hyperosmolar hyperglycemic state (HHS) conditions that develop in patients with type 2 diabetes that often requires hospitalization. The elderly, in particular, are at increased risk for HHS, with overall mortality said to be 10 times higher than diabetic ketoacidosis (DKA). Uncontrolled glucose levels can lead to multiple cardiovascular complications. 2. Respiratory infections are the leading cause of infections in people with diabetes, especially those caused by Streptococcus pneumoniae and influenza virus and are 6 times more likely to be hospitalized during influenza epidemics than patients without diabetes. All recommend antipneumococcal and influenza vaccinations for people with diabetes. 3. Diabetes had a significantly greater risk for severe pneumonia, release of tissue injury-related enzymes, excessive uncontrolled inflammatory responses, and hypercoagulable state associated with dysregulated glucose metabolism compared with persons with no diabetes. Persons with diabetes also had higher levels of biomarkers suggesting an inflammatory “storm” preceding rapid deterioration of COVID-19. Markers of inflammation, including C-reactive protein, erythrocyte sedimentation rate, and interleukin (IL)-6 were also higher in the diabetes group (all P < 0.01). 4. The severity of COVID-19 in diabetes may be hidden by an initial milder presentation. Fewer patients with diabetes experienced fever (59.5% vs 83.2%; P = .002), chills (56.8% vs 71.5%; P = .086), chest tightness (13.5% vs 29.2%; P = .053), and shortness of breath (13.5% vs 27%; P = .089). 6. The ACE2 receptor antagonism has been identified as the receptor for the coronavirus spike protein. By attaching itself to this receptor, SARS-CoV-2 virus is said to reduce expression of ACE2, which, in turn, reduces its protective effects regarding inflammation. This induces hyper-inflammation and other cellular damage, leading to respiratory failure. Chronic hyperglycemia is said to potentiate the effects of downregulating the ACE2 receptor as well as resulting in similar damage.
e. Education, general lifestyle and personal income all influence COVID-19 mortality. Throughout the US, Blacks, make up 13% of the population but 30% of the mortality. Initial studies in Baltimore where 30% are black, brown or poor, show that they made up 75% of the cases and 50% of deaths. This is because of poor access to medical care and methods to prevent spread. A similar situation exists for native Americans and Latinos. There is no evidence that they are biologically or genetically predisposed, but diabetes, hypertension and coronary artery disease are all more common in blacks, Latinos and native Americans. The homeless are also particularly at risk.
Navajo Reservation. With 175,000 residents spread over 27,ooo² miles, this reservation has more deaths per capita than anywhere in the US. It is a food desert with only 13 places to buy any food. 35% of the population don’t have running water, so even hand washing is difficult.
15 million American homes have no running water – municipal districts cut off water for nonpayment of bills. The city of Detroit was the only one reconnecting people during the epidemic. These are mostly poor black and brown people.
f. Longterm care homes. These have seen incredible infection and death rates. Half of all deaths in Canada have been in old age homes. Most residents live in multi-bed rooms, have many co-morbid conditions, are poorly mobile, are frail, dementia is common and the institutions understaffed. Adequate PPE, along with the training to use it properly is rare. Workers may have poor infectious disease training and many work in multiple institutions to get adequate work, thus facilitating spread. Private nursing homes have many more cases than public ones.
Many families, if able, have shown the desire to remove their aged relatives from homes. But leaving often loses the bed even if it is paid for. Returning could occur only once infections are completely controlled. Because of long waiting times, getting back in could take long periods. Families doing this have let their emotional responses override common sense.
g. Prisons. Much attention has been given to prison populations because of rapid contagion in confined spaces. This is especially serious in the US with more prisoners than any other country. Early discharge for non-serious offenders is mandatory.
h. Third World Countries. South Asia is expected to be particularly hard hit, SE Asia and Africa less so. Weak governments, poor safety social nets, poor medical systems and high density populations all play a role.
70% of Africans are under 30, few are old and thus serious illness is expected to be low. African countries are more experienced than anywhere else dealing with epidemics. African countries have been “racing to the top” to see who can institute the most draconian rules as they all locked down very early. 40% don’t have access to adequate water supplies to wash hands etc. There is a locust infestation happening in the Horn of Africa. Economies and supply chains are already fragile. Commodities and their movement are a large part of economies. Family and friends are major social interactions.
Economies will be much more impacted than health.
As of May 2021, death rates in most African countries was 10 to 100 times less likely. this was ascribed to the young age, no seniors in nursing homes, and a more “outside” lifestyle. Most remain completely closed.
i. Refugee camps. In 2020, refugees around the world are at the highest ever – 71 million. They are especially vulnerable due to crowded conditions, malnutrition and lack of any but basic medical care.
Cox’s Bazaar in Bangladesh, home to 850,000 Rohingya from Myanmar and the largest “homeless” population in the world, have received much press.
j. Ignorant religious beliefs that allow congregations to meet (Iran, USA) have been significant methods of spread. Religious groups have had the most difficulty complying with distancing rules. Inciting 2nd Amendment rules that guarantee freedom of association, many churches in the US have been allowed to hold live services over the Easter weekend. Many devout American Christians believe “they are cloaked with the blood of Jesus” and protected from illness.
Muslim countries like Iran have allowed congregation at mosques. In the southern US, many churches have continued holding services especially during Easter held over the April 9-12th weekend.
Easter in the Eastern Orthodox religion occurred over the April 16-19th weekend. The Georgian Orthodox church has ignored all restrictions and acting as if COVID-19 didn’t exist. The Russian Orthodox initially ignored all recommendations, but after many cases occurred, finally closed down churches just before Easter.
4. TREATMENT
In the absence of a proven effective therapy, current management consists of supportive care, including invasive and noninvasive oxygen support and treatment with antibiotics. In addition, many patients have received off-label or compassionate-use therapies, including antiretrovirals, anti- parasitic agents, anti- inflammatory compounds (Ibuprofen was thought to be a problem but proof is lacking and has since been shown to be safe).
This infection will continue to spread until completely eradicated. It is expected that COVID-19 with cycle recurrently until effective prevention is found. This has happened in Singapore where the large population of workers is housed in crowded dormitories.
1. ESTABLISH HERD IMMUNITY
This occurs when a significant percentage of the total population gets the infection and thus develops immunity, limiting spread. For COVID-19, it is uncertain how long this immunity will last or how often the virus mutates (and then requires a new immune response), but experience with other corona viruses suggests that immunity will last.
Infected populations would develop sufficient immunity to prevent a resurgence of the pandemic. The proportion necessary for herd immunity varies with the infectivity of the infectious agent – from as few as 50% to the 80% necessary to control other viral diseases like measles and polio. For COVID-19, in western countries with large old populations, this would produce a dangerous situation as medical services would be quickly overwhelmed and death rates maximal.
Surprisingly, this is the approach adopted in Sweden. Schools, restaurants and most shops remain open. Group size is limited to 50 or less. They believe that it is more important for its citizens to have complete freedom. The world is avidly watching to see how their radical experiment will work.
It is also what will happen in poorly developed 2nd and 3rd world countries with limited resources to both prevent spread and provide treatment. It may be the only way COVID-19 is eventually controlled in the world because of its marked infectivity until an effective vaccine or other practical treatment becomes available. This will require billions of doses.
My personal estimate of the percentage required for herd immunity with covid 19 will be quite high because of its infectivity – at least 80-85% will be necessary, approaching measles. Antivaccers of 15% alone may prevent acquiring this level,
2. DRUGS
a. Hydroxychloroquine (HCQ, Plaquenil). An early small study in France showed that HCQ alone and with azithromycin shortened the time of viral shedding of COVID-19. Based on this one study, clinicians in many countries began using both and multiple randomized trials were initiated.
Several large randomized controlled studies (fourteen to May 18) have since clearly shown HCQ does not help clear or relieve symptoms of COVID-19 and has more side effects. Doses were 1200 mg daily for 3 days followed by 800 mg daily for 2 or 3 weeks. Adverse events occurred in 8.8% of patients in the control group compared with 30% in the HCQ group – diarrhea was the most common.
Citing the first studies, Trump, with zero medical knowledge or common sense, has been the ONLY proponent of using it, completely ignoring his medical experts. “How can it hurt to try it?” “It works in malaria and lupus.” “I have a strong feeling that it will work, probably very well.” It’s been around for 4o years, it’s very safe” What an idiot! His chief medical advisor Dr Fauci had to be placed under armed guard, as he had so many death threats for mildly contradicting the asshole. On May 18, Trump announced that he had been taking HCQ for 10 days (when his valet became positive for COVID) for preventative reasons. He was also taking Azithromycin and zinc. HCQ has been shown to have no effect in preventing COVID and using it may give people a false sense of security and thus not use more effective methods.
On the basis of Trump’s “feelings”, 29 million doses were stockpiled in the US and the run on the drug has affected access for those who need it for their arthritic conditions. For example, on April 14th, a chief of pediatrics at a large American university who had contracted COVID-19, who unbelievably for a medical expert, self-medicated himself with HCQ, got much worse during his 5-day course and had to be admitted to ICU – he survived. He believed (and probably voted for) Trump, believing him rather than best medical advice.
Uses. Hydroxychloroquine has 2 main uses in medicine.
1. Malaria. It is indicated for the suppressive treatment (400 mg once per week) and in acute malaria (800 mg, then 400 mg in six to eight hours and 400 mg for two more days) due to P. vivax, P. malaria, P. ovale, and susceptible strains of P. falciparum. It is not active against the exo-erythrocytic forms.
2. Disease-modifying anti-rheumatic drug (DMARD). It is indicated for the treatment of rheumatoid arthritis, and discoid and systemic lupus by suppressing the immune system, It modifies the underlying disease process, rather than treating the symptoms.
To treat lupus, the adult dose is 400 mg once or twice daily.
Side effects. HCQ typically is very well tolerated with few serious side effects. The most common are nausea and diarrhea, which often improve with time. Less common are rash, changes in skin pigment (such as darkening or dark spots), hair changes, and muscle weakness. A rare anemia can occur in patients with G6PD deficiency or porphyria.
In rare cases, HCQ can affect the retina, more more likely with high doses for many years, in individuals over 60, significant kidney or liver disease, and those with underlying retinal disease. Eye exam are recommended.
Cardiac risk. Chloroquine, HCQ and azithromycin all prolong the QT interval, increasing risk of an arrhythmic death called torsades de pointes (TdP), a potentially lethal polymorphic ventricular tachycardia. Risk is higher if female, in structural heart disease, congenital long-QT syndromes, electrolyte disturbances, hepatic/renal failure and concomitant QT prolonging medications. Azithromycin also increases QT interval increasing risk.
Several hundred million courses of chloroquine have been used worldwide making it one of the most widely used drugs in history, without reports of arrhythmic death under World Health Organization surveillance. Nonetheless, the absence of an active drug safety surveillance system in most countries limits reassurance from these observations.
b. Remdesivir is a nucleotide analogue prodrug that inhibits viral RNA polymerases. It has broad-spectrum activity against several virus families, including filoviruses (e.g., Ebola) and coronaviruses (SARS and MERS). It appears to have a favourable clinical safety profile. It is administered intravenously (200 mg on day 1, followed by 100 mg daily for the 9 days) and thus can only be given in hospital.
In a study published in the NEJM, it was given to patients with confirmed COVID-19 infection who had an oxygen saturation of 94% or on ambient air or on oxygen support.
Of the 53 patients, 22 were in the United States, 22 in Europe or Canada, and 9 in Japan. 30 were receiving mechanical ventilation and 4 extracorporeal membrane oxygenation. 68% had an improvement in oxygen-support class, including 57% on ventilators, all who were extubated. A total of 25 patients (47%) were discharged, and 7 patients (13%) died; mortality was 18% (6 of 34) among patients receiving invasive ventilation and 5% (1 of 19) among those not receiving invasive ventilation.
Preliminary results from the Adaptive COVID-19 Treatment Trial (ACTT), the first clinical trial launched at 68 sites ― 47 in the United States and 21 in countries in Europe and Asia showed that the time to recovery (ie, being well enough for hospital discharge or to return to normal activity level) for remdesivir was 31% faster than for those who received placebo, the median time to recovery was 11 days compared with 15 days for placebo and a survival benefit, with a mortality rate of 8.0% for the group receiving remdesivir and 11.6% for the patients who received placebo.
c. HIV combination drugs like lapinavir-ritonavir are being studied. One study of 199 patients showed no benefit.
f. Broad – spectrum antibiotics. The recommended antibiotic is Azithromycin, a broad-spectrum macrolide-type antibiotic that is very effective in treating a huge variety of bacterial infections from upper respiratory infections (sinus, ear, throat), mycoplasma pneumonia, community acquired pneumonia, sexually acquired infections and skin infections. It has no effect on viruses like COVID-19 but may lessen bronchial secretions and concomitant bacterial infections. Its appropriate use could help in patients with more severe lung involvement, but has side effects (especially when combined with hydroxychloroquine – see above) and should not be used indiscriminately because of increased risk of bacterial resistance. Unfortunately, that is happening in the USA as patients threaten their physicians with legal action if it is not prescribed.
g. Modifying the renin angiotension system. COVID-19 activates the renin-angiotension system causing both endothelial damage in lung tissue and worsening heart failure and hypertension, both more common in men and treated with ACE (angiotension converting enzyme) inhibitors and ARBs (angiotension receptor blockers). Both classes of drug increase ACE2 enzyme, but by different mechanisms. ARBs block angiotensin II, resulting in high angiotensin II levels. ACE inhibitors, but not ARBs, upregulate ACE2 receptors and prevent the enzyme’s uptake by the virus.
A new observational study released on May 19 showed that ACE inhibitors were associated with both a 40% lower risk for COVID-19 hospitalization and death for people over 65 but of no benefit for younger patients or for anyone taking ARBs. What is confusing is why this effect be apparent only in older people?
Both are cheap, widely available, and well-tolerated drugs commonly used to treat hypertension and heart failure.
Smoking has a confounding but profound beneficial effect in COVID. There’s limited evidence that nicotine may down regulate ACE2 expression in the lungs, reducing the receptors by which the coronavirus enters cells.
3. RESPIRATORY SUPPORT
Oxygen in various forms and CPAP are given to people in the hospital with decreased oxygen saturation (less than 94%). It appears that COVID-19 patients are relatively tolerant of lower oxygen levels. Oxygen and CPAP should occur first and ventilators avoided except at a last resort. Mechanical assistance is not without risk. Once respiratory failure has occurred, intubation, complete sedation and ventilators are necessary. But the survival rates of patients on ventilators is very poor with 70-90% dying. Despite all the worry over the availability of ventilators, that has not occurred and more energy was put into ventilators than necessary – instead of supplying PPE and doing more testing.
Budesonide. This relatively cheap inhaled corticosteroid drug used for asthma, alleviates symptoms. It is especially useful for home therapy.
4. VITAMIN D is important to innate immunity and boosts immune function against viral diseases. It can lower inflammation, and this may be relevant to the respiratory response The prevalence of vitamin D deficiency was eightfold higher among those with severe COVID illness compared with those with mild illness. People are encouraged to be outdoors and physically active leading to increased synthesis of vitamin D in the skin.
The recommended dietary allowance of vitamin D is 600-800 IU/daily, but during this period, a multivitamin or supplement containing 1000-2000 IU/daily of vitamin D would be reasonable.
5. PLASMA. Patients who have survived COVID-19 infections develop antibodies to the virus. Drawing their blood, separating the plasma and then infusing it into severely ill patients makes sense to be effective but studies are preliminary.
Cloned antibodies can also be manufactured and then infused into patients.
6. VACCINES. Vaccines will be the major effective way of creating herd immunity. At least 70 different clinical studies were started all over the world in the race to develop an effective vaccine using several different platforms (with different ways of producing an immune response).
Many vaccines are novel in their action compared to previous vaccines. Some insert mRNA sequences into the patients who then manufacture the protein spikes on the surface of the virus and then the body makes antibodies against the protein. These can be scaled up rapidly to produce large amounts of vaccine as they don’t require incubation in eggs and other media.
However, it normally takes 12-18 months to go through the 3 steps of clinical trials to prove safety and efficacy. As of mid April, 3 vaccines had begun human trials – it is possible that one may be available in September. Despite warnings of a potential pandemic, the world has shown how poorly prepared they are. Research into vaccines halted after SARs and MERs and vaccine introduction is expected to be 18 months away instead of the 6-9 months expected if this element of science had been kept active.
Vaccine Manufacture – How Vaccines are Made, and Why it is Hard. Economist.
Nine vaccines against covid-19 have already been approved in one jurisdiction or another, with many more in various stages of preparation. That this has happened within a year of the illness coming to the world’s attention is remarkable. But it is one thing to design and test vaccines. It is another to make them at sufficient scale to generate the billions of doses needed to vaccinate the world’s population, and to do so at such speed that the rate of inoculation can outpace the spread and possible mutation of the virus.
Broadly, there are two ways of making antiviral vaccines. One, tried and trusted, involves growing, in tanks called bioreactors, cell cultures that act as hosts for viruses which are then used in one way or another to make the vaccine in question. Cells grown this way can be of many types—insect, human kidney, monkey kidney, hamster ovary—as can the resulting vaccines. These may be weakened or killed versions of the virus to be protected against, or live viruses of a different and less-dangerous sort that carry a gene or two abstracted from the target virus, or even just isolated target-viral proteins. The point is that the vaccine should introduce into the body, or induce that body to make, something which the immune system can learn to recognise and attack if the real target virus should ever turn up.
The alternative method, developed recently and employed to make the mrna vaccines, such as those of Moderna and Pfizer, that the pandemic has stimulated the invention of, requires culturing cells only at the beginning of the process. mRNA is the substance that carries instructions about how to make a protein from a cell’s DNA to the molecular factories, known as ribosomes, which do the actual manufacturing. In the case of covid-19, the instructions in question generate spike, a protein found on the surfaces of particles of SARS-COV-2, the virus that causes this illness. Suitably packaged and delivered, such mRNA can induce some of the body cells of the inoculee to turn out spike, which the immune system then learns to recognise. To make this type of vaccine you therefore have to generate lots of the relevant mRNA.
That process does indeed start with cells, though they are bacterial cells, rather than those of animals. But it does not end with them. The bacteria used, normally a well-understood species called E coli, have spliced into them a DNA version of the part of the sars–cov-2 genome which describes spike. (Confusingly, as is true of many viruses, sars–cov-2’s actual genes are made of RNA.) The bacteria are then allowed to multiply for a few days before being broken open, their DNA filtered out, and the DNA versions of the spike gene extracted as what is known as a DNA template.
Once purified, this template is mixed with a soup of pertinent enzymes and fed molecules called nucleotides, the chemical “letters” of which RNA is composed. Thus supplied, the enzymes use the templates to run off appropriate mRNAs by the zillion. These are extracted and packaged into tiny, fatty bubbles to form the vaccine.
Both the cell-culture and the mRNA approaches have benefits and drawbacks. The former has the advantage of being well established. Versions of it go back to vaccine-making’s origins. But keeping cultured animal cells alive and healthy is a tricky business. A whole subfield of bioengineering is dedicated to this task. Vaccine-makers who rely on live cultures constantly struggle with yields. Using this method to make a lot of vaccine, fast, is hard.
It was difficulties of this sort that Pascal Soriot, boss of AstraZeneca, cited on January 26th in defence of his firm’s failure to provide vaccine supplies which the European Union claimed it had been promised. AstraZeneca is an Anglo-Swedish company that, in collaboration with Oxford University, created one of the first vaccines to be approved. As Mr Soriot told La Repubblica, an Italian newspaper, “You have glitches, you have scale-up problems. The best site we have produces three times more vaccine out of a batch than the lowest-producing site.”
Maximising a bioreactor’s yield is as much an art as a science. The underlying health of the cells involved matters. So do environmental conditions at the manufacturing site. That AstraZeneca has not been able to meet its own production targets shows how hard it is to predict when the right balance of biology will be found. The company says it can take six to nine months to start a production site up from scratch, and that even this timetable is possible only by working with experienced partners and at an accelerated pace. At the moment, AstraZeneca is working with 25 manufacturing organisations in 15 countries to make its vaccine.
Producing mRNA vaccines at scale has problems, too. The biggest is how to protect the mRNA molecules both from the environment they must travel through in order to reach the arm of their recipient, and from the recipient’s own body, which will attack them as they journey to the ribosomes which will transcribe them.
Protection from the environment is mainly a matter of having a strategically located set of refrigerators, known as a cold chain. Protection from the body, though, is where the fatty bubbles come in.
Production of these bubbles was a cottage industry before the pandemic. A small Austrian firm, Polymun Scientific, is one of just a handful that can make them. Their main previous use was in niche cancer treatments. Scaling up their production, which is happening right now, has never been done before and adds uncertainty to the continued supply of mRNA vaccine.
There are other bottlenecks, too. In particular, the factories in which vaccines are made must be built to a high standard, known as GMP, for “Good Manufacturing Practice”. There is currently a shortage of GMP facilities. Andrey Zarur, boss of GreenLight Biosciences, a firm in Boston that is developing an mrna vaccine, says his company has employees whose entire job, at present, is to work the phones trying to find GMP facilities in which to make their vaccine. There is, though, nothing available. He is therefore looking to buy firms whose vaccine candidates have turned out not to work, simply in order to acquire the facilities in question.
Supplies of raw materials such as nucleotides are also tight. According to Dr Zarur, Thermo Fisher, an American chemical-supplies company, has spent $200m on a new facility in Lithuania to make these molecules, though the firm itself would not confirm this.
On top of all this, the transport and distribution of vaccines once they have been made presents yet further challenges, and concomitant potential for hold ups. Vaccines must be stored in special non-reactive glass vials. Some, such as the current version of Pfizer’s mrna vaccine, must also be kept at extremely low temperatures, though that problem may go away soon. Drew Weissman, one of the inventors of mRNA-vaccine technology, says producers are now testing shots which are stable for three months when kept at 4°C.
Once supply chains for both cell-culture and mrna vaccines have been scaled up, and bottlenecks unblocked, the manufacturing processes may face a different test—how quickly they can produce new vaccines to deal with new viral variants as these emerge. The continued efficacy of approved vaccines against such variants is not guaranteed, and it may be necessary to make others.
Here, the mRNA approach may have an advantage. Its production systems will require a simple tweak—the dropping in at the start of a DNA template describing the new variant’s spike protein. Cell-culture systems, by contrast, will have to be rebuilt to some degree for every new variant they aim to vaccinate against.
Scale models. Producers, such as those in China, who use older-fashioned cell-culture techniques, will have to recalibrate their entire operations. Newer systems, like AstraZeneca’s, which use cells specially designed so as not to be influenced by the new version of the spike gene in the viruses they are carrying, should be able to get on track in the time it takes to start a culture from scratch—about a month. For mRNA systems, Drs Weissman and Zarur say it would take a couple of months to go from new variant to large-scale vaccine production. If variants resistant to the current crop of vaccines do evolve, then that speed and certainty in making new vaccines to combat them will be essential.
The medicine is the message
Covid-10 vaccines have alerted the world to the power of RNA therapies.
And the molecule has more tricks up its sleeve.
March 27, 2021 Economist
Molecular biology is not a popularity contest. But if it were, it would be a partisan one. The evolutionary biologists would pledge their allegiance en masse to dna. The sequences contained in its regular coils knit together the stories of almost all life on the planet. Pharmacologists, being of a more practical bent, would instead vote for proteins. Proteins are not about sequence, but about shape; their complex, irregular outlines, and the ways that they can change, allow them to do almost all of the biological work that gets done in cells. And it is thanks to the way that particular drug molecules fit into those shapes that almost all drugs have their effects.
There would be only a small following for ribonucleic acid (rna), widely seen as a helpmeet molecule. It could be argued that the production of rna is dna’s main purpose; it is certainly true that the production of proteins would be nowhere without it. But it is a backstage operator, not a star; hewing wood and drawing water, hard working but hardly glamorous, appreciated only by devotees.
Or at least that was the case until vaccines made of rna started giving protection against covid-19 to millions of people around the world every day. Now Cinderella has gone to the ball. Not only are rna vaccines being considered for all sorts of other diseases, some of which have yielded to no other approach; other pharmaceutical uses of rna look set to come into their own, as well. The way molecular biology is applied to medicine seems to be in the throes of revolution.
Incarnation Incarnate. The great unifying truth of molecular biology, uncovered during the intellectual revolution which followed the discovery of dna’s double-helix structure, is the way in which the worlds of shape and sequence are linked. The shape of a protein depends on the intricate way in which the chain of amino acids of which it consists is folded up. That depends in turn on the order in which amino acids of different types are strung together on that chain. And the order of the amino acids is a crucial part of the genetic information stored in the dna sequences of the cell’s genome.
The transfer of information from the staid archival form it takes in the genome to its active physical instantiation in the machineries of the cell depends on rna, a molecule in which both sequence and shape play crucial roles. The gene sequence is first copied from dna to rna; that rna transcript is then edited to form a molecule called a messenger rna, or mrna (see diagram).

The end of the mrna molecule is formatted into a distinctive shape which is recognised by ribosomes, complex pieces of machinery composed of dozens of proteins draped around another set of rna molecules. With the help of yet more rna molecules—little ones called trnas which stick to the mrna sequence three letters at a time—the ribosome translates the genetic message into the protein it refers to by creating a chain of amino acids as it moves along the message.
This is the mechanism exploited by the rna vaccines developed by BioNTech, a German biotechnology company based in Mainz, and Moderna, an American one from Cambridge, Massachusetts, against sars-cov-2, the virus which causes covid-19. The companies mass produce the rna sequence describing the distinctive “spike” protein, which studs the outer membrane of the virus, formatted so as to look like a natural mrna. These rna molecules, wrapped in little fatty bubbles called liposomes are injected into patients, where the liposomes smuggle the mrna into cells. Ribosomes pick up on the mrna format and read the sequence, thus producing the spike protein. The immune system learns to recognise the spike which the vaccinated cells are producing and stores away the memory of how to do so. This allows it to mount a swift response if it later comes across the same protein on the surfaces of viral particles and infected cells.
This ability to get cells to churn out proteins for which their dna contains no genes is, in itself, enough to open up swathes of new therapeutic territory. But it is not the whole story. Cells make vast amounts of rna that does not describe proteins. Its ability to recognise specific genetic sequences makes it useful for all sorts of processes, including turning the translation of genes on and off. Its ability to fold itself into particular forms—hairpins, loops and the like—makes it good at interacting with proteins.
This alphabet soup of rnas (see table) seems to function a bit like a computer’s operating system, mediating the relationship between the cell’s hardware and its software. Many of the details of how this works remain obscure. But some are understood well enough for a lot of brainpower and money to have been poured into attempts to hack the operating system for therapeutic purposes.

These abilities should enable drugmakers to head upstream from the proteins whose shapes they have long studied into the realms of sequence. Where previously they targeted proteins which were already present, now they can in principle target the processes which control which proteins get made in the first place, adding helpful new ones to the roster and crossing harmful old ones off. There are rna-based drugs in clinical trials for the treatment of cancer, heart disease and numerous inherited disorders—as well as brain diseases such as Alzheimer’s and Parkinson’s.
Moreover, rna’s mixture of sequence and shape means that in many of these areas the once-haphazard process of drug discovery, long dependent on matching the shape of small synthetic molecules to the crannies and crevices of the proteins they targeted, can itself be systematised. A sequence which recognises, or forms a part of, one gene can be switched out for a sequence tailored to another. When what an rna drug does depends on its sequence, its target and action can be modified by the click of a mouse.
The medicine is the message. Both the firms with mrna vaccines on sale had other vaccines in the pipeline before covid-19 struck. It is part of the appeal of the technology that they were able to turn on a sixpence and refocus their efforts on sars-cov-2 as soon as the sequence for its spike gene was released last January. Now they are both getting on with what they had planned beforehand. Moderna is looking at vaccines to fend off infection by cytomegalovirus (a herpes virus which causes neurological problems in newborns), three lung viruses which cause respiratory disease in young children and Zika, a mosquito-borne virus found mainly in the tropics. BioNTech is focusing more on developing vaccines, and other treatments, with which to treat a wide range of cancers.
Cancer cells tend to have peculiar constellations of proteins on their surfaces, including both normal ones that are overexpressed and, more intriguingly, mutant forms peculiar to the development of that tumour. Comparing the genes expressed in a patient’s healthy cells with those used by their tumour cells reveals which mutant proteins the cancers are producing; mrnas for those proteins can then be incorporated into a vaccine.
Produced as a result of vaccination, the proteins can engender a vigorous immune response the cancer itself does not—part of being a successful tumour is deploying mechanisms that stop the immune system from coming to grips with you. According to Ozlem Tureci, BioNTech’s co-founder, the firm has 500 patients enrolled in clinical trials for cancer. Moderna is pursuing similar ideas.
BioNTech is also testing mrna vaccines aimed at overexpressed but unmutated proteins. Moderna, meanwhile, is looking into vaccines that train the immune system to recognise proteins created by common mutations in kras, a gene implicated in about 20% of human cancers. CureVac, based in Tübingen, an mrna firm which also has a sars-cov-2 vaccine in trials, is conducting trials of a vaccine for non-small-cell lung cancer.
Vaccination is not the only way that mrna injection might fight viruses and tumours. The technique could also be used to get cells to produce therapeutic proteins that are currently administered through injection or infusion: interleukins and antibodies. Designer antibodies are a massive faff to make in industrial quantities; getting patients’ cells to take on the manufacturing duties instead would be a great step forward if it proved practical.
There are many other sorts of proteins which can be stimulated to therapeutic effect. A project on which Moderna is collaborating with AstraZeneca, a pharmaceutical giant, delivers the mrna for a protein which encourages the regrowth of blood vessels. The idea is that the therapy, now in phase 2 clinical trials, could stimulate the growth of new cardiac blood vessels after heart attacks.
Getting the body to produce a protein it needs just for a short while—an antibody, say, or a growth factor—is one thing. But what about a protein that it needs on an everyday basis, but lacks the gene for? Such genetic diseases have always been the most obvious targets for gene therapy—treatments which add a missing gene to a patient’s cells, or repair a broken one, thus allowing them to make a protein they have hitherto lacked. But at least some such conditions might instead be treated with mrna. Inserting a gene might be more elegant—but getting it in the right place and regulated in the right way is challenging. If mrna treatments get the job done, they might offer a nice alternative.
There are thus mrna treatments being studied for phenylketonuria, a metabolic disorder which requires sufferers to restrict their diets for their entire lives; glycogen-storage disease, which enlarges the liver and kidneys and stunts children’s growth; and propionic and methylmalonic acidemias, two illnesses in which the body cannot properly break down proteins and fats. All are conditions that gene therapists are looking at, too.
That BioNTech, Curevac, Moderna and some others now have all these projects on the go is largely down to the fact that they have spent many years developing the basics of their platforms. Many hurdles had to be crossed before they could get cells to accept and act on messages from beyond; the rna had to be subtly toughened up so that it would not itself fall prey to the immune system or get dismantled inside cells; the right lipids had to be found for delivery, sometimes tailored to particular tissues like those of the liver or lymph nodes. The potential inherent in the idea meant that their work was not completely ignored; in 2018 Moderna’s ipo valued the company at $7.5bn, a record for the biotech sector. But biotechnology has a long history of proving biology to be messier and more contrary than those seeking to exploit its loopholes expect.
Stop Making Sense. Scepticism was also warranted, it seemed, by the fact that messing around with rna had been through bursts of popularity before. One of the very oldest companies in the field, Ionis Pharmaceutials (known as Isis until that name was appropriated by a would-be caliphate) was founded in 1989. Its intention, then and now, was not to make use of mrna, but to hobble it.
The sequence of an mrna molecule carries the same information as can be found in the gene which served as its template; but thanks to the way rna is made it carries it in a complementary way. Where the dna has a letter called C for cytosine, the rna will have G for guanine; where the rna has a C the dna will have a G, and so on. Complementary strands stick together; that is what keeps dna molecules paired up in double helices. If you introduce an mrna to a molecule with a complementary sequence the two will stick together, too, rendering the mrna useless (see bottom deck of diagram above).
Again, getting the neat idea to work in ways that helped proved hard. It took Ionis a quarter century to start getting its “antisense” drugs to market on a regular basis. It now has three: nusinersen, approved in America in 2016 and Europe in 2017 for use against childhood spinal muscular atrophy, a muscle-wasting illness; inotersen, approved in 2018 for hereditary transthyretin-mediated amyloidosis (hattr), which damages the peripheral nervous system; and volanesorsen, approved in Europe in 2019, which lowers levels of triglyceride fats in the blood of people with a metabolic error that makes them far too high.
Ionis currently has a further 37 antisense molecules in clinical trials for conditions including Huntington’s disease (a study being carried out in collaboration with Roche, a large Swiss pharma company); amyotrophic lateral sclerosis, Alzheimer’s disease and Parkinson’s disease (in collaborations with Biogen, a specialist in treatments for neurological disease); beta thalassaemia, a blood disorder similar to sickle-cell anaemia; and cystic fibrosis.
The firm is also developing, in collaboration with Novartis, another Swiss company, a way of reducing levels of lipoprotein(a), a particularly damaging form of low-density-lipoprotein (ldl) cholesterol. Lipoprotein(a) levels are untreatable with existing medicines; Pelacarsen, as the drug is known, is in phase 3 clinical trials to see if it can change that.
Unlike molecules of mrna, which can tolerate only a small amount of chemical tinkering before becoming ribosome-unfriendly, antisense molecules can be tweaked quite a bit, and thus made long-lasting. Ionis’s researchers have worked out how to stabilise them so that they will hang around inside cells for months. This is important because most of Ionis’s targets are chronic diseases that require continuous treatment. The fewer injections per year the better.
While biotech companies were beavering away at antisense molecules in the 1990s, researchers elsewhere discovered that nature had a similar technology of its own: gene silencing, a process guided by small interfering rnas (sirnas). The early 2000s saw a gene-silencing biotech boom led by Alnylam, founded in Cambridge, Massachusetts in 2002, and Sirna Therapeutics, which got going in San Francisco the following year.
Established pharma companies, including Abbott, Merck, Novartis, Pfizer, Roche and Takeda, waded in, too, with Merck buying Sirna for more than $1bn in 2006. For almost a decade, attention and money were showered on the field. But though there were many promising leads, they failed to turn into drugs. By the early 2010s it seemed that the party was over.
Nonlinea, nonvisual. Alnylam, though, kept dancing. In 2014 it bought what was left of Sirna from Merck for a knock-down price. It launched its first product, patisiran, a treatment for hattr, in 2018. It now has two others, givosiran and lumasiran, which also address rare genetic disorders.
A fourth substance developed using its technology has broader appeal. This is inclisiran, developed to treat an inherited disorder that pushes the concentration of ldl cholesterol in the blood to dangerous levels; around 30m people worldwide suffer from it. A firm called the Medicines Company licensed Inclisiran from Alnylam to bring it to market. With approval looking likely (it was given in Europe late last year) Novartis bought the Medicines Company for $9.7bn in January 2020.
According to Akshay Vaishnaw, Alnylam’s head of r&d, the firm has another 14 sirna drugs in clinical trials. These including potential treatments for haemophilia, hepatitis B and recurrent kidney stones. Arrowhead Pharmaceuticals, of Pasadena, California, has eight potential sirna drugs in trials, including one directed at cystic fibrosis. Dicerna Pharmaceuticals, of Lexington, Massachusetts, has three.
These sirnas work by straddling the worlds of shape and sequence. Their shape fits them into a group of proteins called an rna-induced silencing complex (risc). But a bit of the sirna is left sticking out of this complex; this tail contains a sequence complementary to that of the rna to be silenced. When sirna and mrna meet, the proteins in the risc chop the messenger to pieces. (A conceptually similar mechanism for the rna-guided protein-executed chopping up of genes found in bacteria is the basis of the crispr tools now revolutionising gene editing.)
In plants and invertebrates the natural function of the sirna mechanism is clear: cutting up mrnas associated with viruses. They do not seem to serve that function in vertebrates, and no one is quite sure what they do instead. But that does not stop them from looking like promising drugs.
So do another set of rnas associated with riscs: micro-rnas, which use their complementary sequences not to destroy mrnas but to regulate them. The human genome seems to contain about 2,600 of these mirnas, and they are thought to be involved in regulating the rate at which about 60% of the genes describing proteins get transcribed. Several look like promising therapeutic targets.
Since the active bit of an mirna is a single-stranded sequence-specific tail, the obvious way to target them is with antisense. Regulus Pharmaceuticals, a firm that started life as a collaboration between Ionis and Alnylam, is trying to develop antisense molecules aimed at mirna-21 to treat two kidney-related genetic conditions in which that mirna plays a role. When you start targeting mirnas, though, things get positively baroque. Santaris Pharma, a Danish firm, has developed Miravirsen, an antisense suppressor for mirna-122 which the hepatitis C virus uses for its own unhelpful ends. The drug has now been taken on by Roche.
The innovation continues. Mina Therapeutics, a startup in London, is working on the potential of sarnas, which activate genes which otherwise stay silent. Others are investigating systems for “self-amplifying” mrna drugs. These mrnas would inveigle a cell’s ribosomes into producing not just the protein that was meant to be delivered, but also a second protein, called rna-replicase, which would make more of the mrna, thus leading to even more protein being expressed. There is surely further cleverness to come.
Could be so exciting

Even if only a fraction of these possibilities pan out it looks certain that, in popularity contests to come as in stockmarkets today (see chart), more people will be plumping for rna. Their support will be welcomed by the small band of biologists with an interest in the very earliest history of life that has long formed the discerning core of the molecule’s following. Life needs both a way of doing things in the now—catalysing the reactions on which its metabolism depends—and of passing information into the future. Of the molecules known today only rna, in its shape-and-sequence versatility, can do both those things, dealing with the needs of the everyday at the same time as encoding instructions for its own reproduction in the form of a legible sequence. This suggests to many that early life spent some time in an “rna world” before the division of labour allocated doing things to the proteins and storing data to dna, reducing rna to a supporting role in the world it had created.
The application of rna has met many obstacles over past decades, and the fact that it has proved itself in vaccines does not mean it will not meet more in the future. But it does seem that medicine now has a way to target drugs not just at proteins, but at the processes that make them, and that opens up new realms of possibility. The next rna world awaits.
6. SMOKING and NICOTINE. Common sense indicates that smoking would significantly increase risk of pneumonia as smoking adversely affects every aspect of lung function. However, in China, where 50% of men smoke, 13 studies with nearly 6,000 hospitalized COVID-19 patients, the rate of smokers ranged from 1.4% to 12.6%. In the US, where 14% of the country smokes, in 7,000 hospitalized patients, about 1.3% were current smokers and 2.3% were former smokers.
In France, where 34% of its citizens smoke, among 350 people admitted to the hospital, about 4.4% were regular smokers. In late April, a team of French researchers began a clinical trial to test whether nicotine patches may be effective against COVID-19.
There’s limited (and somewhat conflicting) evidence that nicotine may be able to down regulate ACE2 expression in the lungs, reducing the receptors by which the coronavirus enters cells. No studies recorded e-cigarette use.
Nobody would suggest to start smoking – it is the worst thing one could do for their health. But these studies suggest that taking nicotine in some form may offer significant protection, or for those who could easily stop, start smoking now.
ECONOMIC IMPACTS
Possibly the greatest impact of COVID-19 will be economic especially in third world countries with already fragile economies. Wealthy western countries (especially ones that can print their own money) will even be tested. It is predicted that the repression that will result may be the worst since the Great Depression of the 1930s.
The economic and social costs of lockdowns are enormous: estimates from the OECD suggest that every month of pandemic-related restrictions will shrink the economies of advanced countries by two percent. France, Germany, Italy, Spain, the United Kingdom, and the United States will see their economies shrink by more than 25 percent within a year. Unemployment is rising to levels unheard of since the 1930s—fueling political backlash and deepening social divisions.
Lockdowns are simply not sustainable for the amount of time that it will likely take to develop a vaccine. Letting up will reduce economic, social, and political pressures. It may also allow populations to build an immunity that will end up being the least bad way of fighting COVID-19 in the long run.
The justification for general lockdowns grows weaker and weaker. Even in places like the United States and the United Kingdom, where the pool of at-risk people is much larger, the cost of protecting these people is much lower than forcing everyone to stay home.
As the pain of national lockdowns grows intolerable and countries realize that managing—rather than defeating—the pandemic is the only realistic option, more and more of them will begin to open up. But at the end of the day, increased—and ultimately, herd—immunity may be the only viable defence against the disease, so long as vulnerable groups are protected along the way.
This is despite most western countries introducing massive spending bills to try to save businesses and prevent the economic effects of massive unemployment. All but essential businesses (grocery stores, pharmacies, gas stations, health care facilities, liquor stores) have closed their doors and laid off their employees.
Unemployment is rampant everywhere – in the USA, 34 million had lost their jobs prior to the second week of May. In the Great Depression 8 million (25% of employable people) lost their jobs but it took two years to occur in the 1930s.
Countries slow to impose rules have been the most impacted (Italy, USA, Spain, UK, Iran, Russia). And countries that instituted early rules (China, Singapore, Hong Kong, Taiwan, South Korea) saw early control despite being densely populated. The effect in the USA will be devastating as Trump ignores his medical experts, and makes rules stressing economic recovery. If the most powerful economy in the world has problems, think about 2nd and 3rd world countries.
Virtually every government in the world has closed its borders, but supply chains are being kept intact in Europe and North America. Huge segments of the population are under stay at home orders. Working from home and use of video conferencing apps like Zoom has sky rocketed. Small business have been especially hard hit, with restaurants closed but still offering takeout. Large corporations like airlines likewise have been severely impacted.
Tourism has completely ground to a halt and countries dependent on tourism are severely impacted (Maldives, SE Asia). Large numbers of foreigners are trapped in countries not their home. Most well off counties have organized charter flights to bring back their citizens. Obvious foreigners have experienced violence as they are perceived to be the ones who have brought the virus.
Oil prices have hit all time lows, decreasing form $63 in January to $2 on April 20 and May futures negative for the first time at -$37. This was initiated by a pricing war between Russia and Saudi Arabia but with the onset of COVID-19, demand for oil has plummeted. Oil companies are running out of places to store oil and some have even resorted to paying to take the oil off their hands.
Meat processing plants have been out of the largest sources of outbreaks. The Cargill plant in High River, Alberta – that processes 4500 animals per day, and supplies a third of Canada’s beef – has closed along with many others. Poultry and pork processing has also been impacted. Worries about the food supply are warranted. Trump has mandated that meat processing plants remain open.
Health impacts. In western countries all nonessential health services have been cancelled – elective surgery and 400 clinical trials were put on hold in the USA. But in countries with good public health measures, this has resulted in thousands of empty beds. Elective surgery has huge backlogs and patients waiting for cancer surgery have been left hanging.
As this pandemic progresses, economic effects are much more important the the disease and death rates. In several western countries with responsible populations, total death rates hardly changed from pre pandemic times, as true death rates are only about 1% when all the asymptomatic infected people are counted for.
SOCIAL IMPACTS
In the USA, with the most cases and deaths, response to the pandemic has been slow. 16 million Americans had lost their jobs in the 3 weeks prior to April 13 (26.5 million in 5 weeks before April 24 and 33 million by early May which is 15% of the employed population) and along with that, their health insurance. The need for a universal health care plan has never been more important.
Unemployment has caused massive stress. Many more are working at home. Social distancing and stay at home orders keep people in their homes for unusually long periods creating all sorts of stress. Cooking and baking bread are immensely popular – it is difficult to buy flour or yeast. Hand sanitizer, toilet paper and staples like bread, rice and pasta are not on shelves. Nobody can get their hair done and roots are growing in.
Couples now living together 24/7 can produce stress. Spousal abuse and divorces have increased. Alcohol abuse has increased facilitated by liquor stores declared an essential service.
All schools have closed and now parents have to home school and deal with children cooped up inside the house. Only the wealthy have good access to online education that is still available. The economic gap will only increase.
Racism against Orientals has escalated (all people anyone who appear Chinese are involved – most people cannot differentiate between Japanese, Koreans, Mongolians, and SE Asians). They are the ones responsible for the enormous increase in gun sales in the US. Even racism against blacks is a problem in China as Guanzhou has a large Nigerian population.
Nursing homes are especially impacted. Besides the high death rates, they are locked down and families not allowed to visit causing stress. People are dying alone. Funerals cannot be attended. Crematoriums in New York are completely overwhelmed.
The food supply is threatened everywhere. Lockdowns prevent transportation. Meat will be especially impacted as processing plants close. Food prices have increased significantly in the US. The Navajo reservation in Arizona/Utah and New Mexico are food deserts with only 13 stores for 175,000 inhabitants spread over 27,000 miles² and, like most Indian communities are selectively more impacted.
Animals are appearing on the vacant streets. Elephants, leopards and tigers have been seen patrolling Indian streets.
Pollution levels around the world are improving because of decreased traffic.
We should all consider our Advance Health Directives to help our loved ones make informed decisions especially if mechanical ventilation is required. Death rates are high. I personally don’t want to be intubated, heavily sedated, unable to see my family and friends and would consider “do not resuscitate” orders.
Since Trump has been president over the last three years, much of what the press and media holds dear has been threatened – democracy, civility, truth. This US administration is establishing new norms of behaviour. Anger and cruelty disfigure public discourse and lying is commonplace. Truth is being chased away.
Rampant disinformation, partisan news sources and social media’s tsunami of fake news is no basis on which to inform the public in 2020. The need for a robust, independent press has never been greater – fact-based reporting that offers public scrutiny and oversight.
COVID AROUND THE WORLD
China. It appears that the local Wuhan, China government did try to cover up the infections. The Dr who first alerted about the suspicious cases of an unusual pneumonia, demonstrates some of this. But when the national Chinese government understood the scope of the infection, they immediately kept WHO up to date and instituted draconian measures to control it. Extensive testing resulted in anyone with the infection to be quarantined in closed spaces. It is amazing that China was able to completely control the infection in a country of 1.4 billion. The province was locked down for 74 days.
The insinuation that it came from a Chinese lab has no evidence and suggesting it has been a political play of Trump. It is also one of his nefarious methods to deflect blame for his inadequate response.
A second small reoccurrence in Wuhan on May 13 has resulted in another lockdown. The Chinese government have proposed they will test all 11 million citizens of the city.
Other small relapses occurred in the northeast next to the Russian border.
WHO. The World Health Organization has not done a good job in previous epidemics. They were slow to react to the Ebola epidemic in West Africa, but have done an exceptional job with COVID-19 by issuing warnings on January 20, 23 and the pandemic warning on January 30 that was ignored by most of the world. Trump has defunded WHO, again as a ploy to deflect blame.
World. Singapore had a relapse originating in dormitories for the thousands of domestic workers. South Korea has had a relapse originating from a single asymptomatic man who visited several night clubs on one night. Both these were in early May after having no new cases for weeks and easing of stay-at-home rules.
Death rates grow. As of mid May, the countries with the highest rates in Europe are Great Britain, Italy and Spain, all with about 30,000 deaths. Russia had the second most cases after the US. The US leads the world with the most cases and deaths of 84,000.
Sweden – striving for herd immunity. Rather than declare a lockdown or a state of emergency, Sweden asked its citizens to practice social distancing on a mostly voluntary basis. Swedish authorities imposed some restrictions designed to flatten the curve: no public gatherings of more than 50 people, no bar service, distance learning in high schools and universities, and so on. But they eschewed harsh controls, fines, and policing. Swedes have changed their behaviour, but not as profoundly as the citizens of other Western democracies. Many restaurants remain open, although they are lightly trafficked; young children are still in school. It has been projected that the city of Stockholm could reach herd immunity as early as this month.
Sweden has won praise in some quarters for preserving at least some semblance of economic normalcy and keeping its per capita death rate lower than those of Belgium, France, Italy, Spain, and the United Kingdom. Swedish deaths per 1m people: 380 – that’s lower than France (429), Belgium (790), Italy (532), Spain (594) but not the Netherlands (336), the U.S. (284), or Germany (98). It has been criticized for failing to protect its elderly and immigrant populations. People receiving nursing and elder-care services account for upward of 50 percent of COVID-19 deaths, in part because many facilities were grievously slow to implement basic protective measures such as mask wearing. Immigrants have also suffered disproportionately, mainly because they are poorer on average and tend to work in the service sector, where working remotely is usually impossible.
The country’s intensive care units have not been overrun, and hospital staffs, although under strain, have at least not had to juggle additional childcare responsibilities because daycares and lower schools continue to operate.
The economic and social costs of lockdowns are enormous: estimates from the OECD suggest that every month of pandemic-related restrictions will shrink the economies of advanced countries by two percent. France, Germany, Italy, Spain, the United Kingdom, and the United States, according to the OECD, will see their economies shrink by more than 25 percent within a year. Unemployment is rising to levels unheard of since the 1930s—fueling political backlash and deepening social divisions.
Lockdowns are simply not sustainable for the amount of time that it will likely take to develop a vaccine. Letting up will reduce economic, social, and political pressures. It may also allow populations to build an immunity that will end up being the least bad way of fighting COVID-19 in the long run.
Sweden’s approach to COVID-19 reflects the country’s distinctive culture. In particular, reliance on official recommendations and individual responsibility may not travel well beyond Scandinavia. Sweden is a special country characterized by high levels of trust—not just between people but between people and government institutions. Swedes are also generally healthier than citizens of many other countries. It is also surrounded by countries doing a good job at keeping things under control.
The justification for general lockdowns grows weaker and weaker. Even in places like the United States and the United Kingdom, where the pool of at-risk people is much larger, the cost of protecting these people is much lower than forcing everyone to stay home.
As the pain of national lockdowns grows intolerable and countries realize that managing—rather than defeating—the pandemic is the only realistic option, more and more of them will begin to open up. But at the end of the day, increased—and ultimately, herd—immunity may be the only viable defence against the disease, so long as vulnerable groups are protected along the way. Whatever marks Sweden deserves for managing the pandemic, other nations are beginning to see that it is ahead of the curve.
For the complete article, see Sweden.